Excerpt from: The Pharmaceutical Journal, 24 Sep 2020, By Michael Dowdall & Kristoffer Stewart
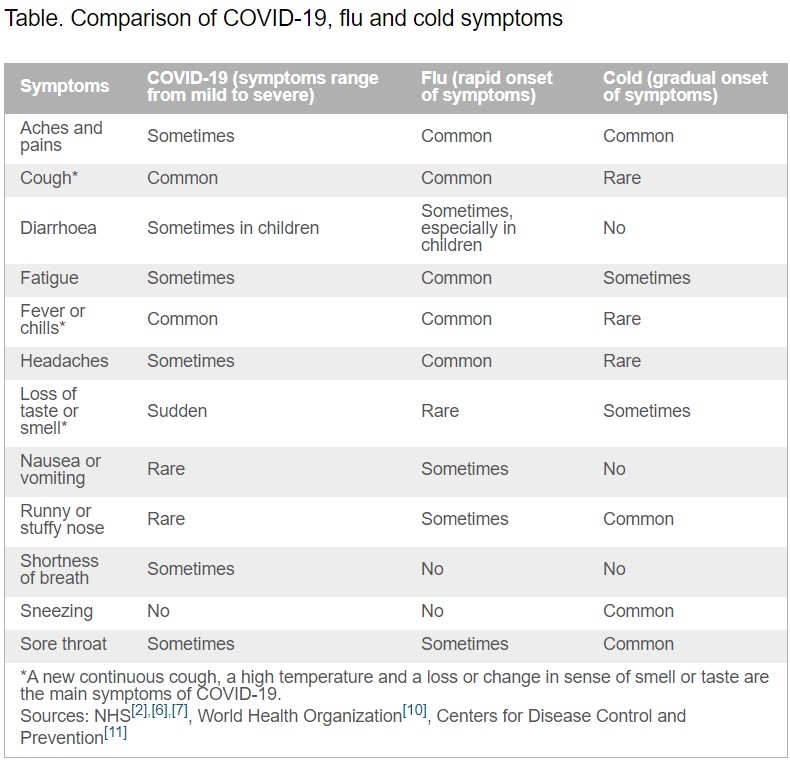
Cold and flu share some symptoms and, if managed effectively, are often self-limiting and resolve within a couple of weeks in people without pre-existing conditions. However, some of their symptoms are similar to those seen in COVID-19 infections, which will present a challenge for healthcare professionals. Below is an overview of the main differences between the symptoms for cold, flu and COVID-19.
COVID-19
Symptoms
The novel coronavirus SARS-CoV-2, commonly referred to as COVID-19, typically causes mild upper respiratory infections.
The main symptoms include:
- A high temperature — the skin feels hot to touch on the chest or back;
- A new, continuous cough — coughing a lot for more than one hour, or three or more coughing episodes in 24 hours (if a patient usually has a cough, it may be worse than usual);
- A loss or change in sense of smell or taste.
Most people with coronavirus will have at least one of these symptoms, with the severity ranging from mild to severe
Colds
Symptoms
A cold is caused by a mild viral infection of the nose, throat, sinuses and upper airways.
Children aged under six years are at greatest risk of colds, but healthy adults can also expect to have two or three colds annually.
Symptoms usually appear gradually and include:
- A sore throat;
- A blocked or runny nose;
- Sneezing;
- A cough;
- A raised temperature.
Generally, patients may feel unwell but are able to continue daily activities as normal.
More severe symptoms, including headache and aching muscles, can also occur, although these are generally associated more with flu. Symptoms usually resolve within one to two weeks.
Influenza
Symptoms
Flu symptoms typically come on very quickly (within a few hours) and tend to be more widespread than those seen in a cold. These may include:
- A sudden fever – a temperature of 38°C or above;
- An aching body;
- Feeling tired or exhausted;
- A dry cough;
- A sore throat;
- A headache;
- Difficulty sleeping;
- Loss of appetite;
- Diarrhoea or stomach pain;
- Feeling sick and being sick.
The symptoms are similar for children, but they can also experience pain in their ear and appear less active. Patients with flu will likely describe feeling exhausted and too unwell to carry on daily activities as normal.
Red flags
Patients may require referral if:
- Sudden chest pain, shortness of breath, or difficulty breathing is experienced;
- There is blood in their sputum;
- They have cold, clammy, or pale and mottled skin, or their lips turn blue;
- They become confused;
- They are difficult to rouse;
- They have little or no urine output;
- A new, severe, non-blanching rash develops;
- Their cold or flu symptoms worsen or do not improve within 14 days.
Patients with long-term conditions or with weakened immune systems may require referral to their physician.
Children or babies aged under five years who seem very unwell or whose condition is worsening should be referred to urgent care immediately.
Important infection control and self-care measures
Infection control
- Wash hands often with warm water and soap for at least 20 seconds;
- Avoid touching your nose, eyes and mouth to prevent virus entry;
- Use tissues when you cough or sneeze and throw these away as quickly as possible;
- Wear a face covering in enclosed spaces or where the two-metre social distancing rule cannot be maintained.
Self-care measures
- Maintain fluid intake;
- Drink hot drinks;
- Gargle salt water to relieve a sore throat;
- Take time to rest;
- Stay at home and recover, normal symptom durations
are:
- Sore throat: 7–8 days;
- Common cold: 14 days;
- Cough or bronchitis: 21 days
Source:
The Pharmaceutical Journal, PJ September 2020 online, online | DOI: 10.1211/PJ.2020.20208379