Study Warns of Diabetic Ketoacidosis With SGLT2 Inhibitors in T2D – Doubled risk compared with DPP4 inhibitors
The newest class of drugs for treating type 2 diabetes carries a greater risk for diabetic ketoacidosis compared to other classes of drugs, a new study suggests.
Newly initiated use of an SGLT2 inhibitor was associated with a roughly twofold greater risk of diabetic ketoacidosis versus new initiation of a DPP4 inhibitor (HR 2.2, 95% CI 1.4 to 3.6), according to Michael Fralick, MD, of Brigham and Women’s Hospital, and colleagues.
Findings were similar in an unadjusted model, while hospitalization for diabetic ketoacidosis (DKA) within 180 days of treatment initiation was around two-times higher with use of an SGLT2 inhibitor compared to a DPP4 inhibitor (4.9 events per 1,000 person-years versus 2.3 events per 1,000 person-years; HR 2.1, 95% CI 1.5 to 2.9).
The findings were published as a letter in The New England Journal of Medicine.
Following twenty case reports of diabetic ketoacidosis with this class of drugs, the FDA issued a warning in May 2015, and announced required label changes later that year after over 70 cases of ketoacidosis were reported.
In June 2016, the American Association of Clinical Endocrinologists and American College of Endocrinology published a position statement in Endocrine Practice stating that “DKA occurs infrequently and that the risk-benefit ratio overwhelmingly favors continued use of SGLT-2 inhibitors with no changes in current recommendations. However, DKA diagnosis may be missed or delayed due to atypical presentation involving lower-than-anticipated glucose levels or other misleading laboratory values,” ultimately recommending additional research on this association.
Fralick explained in a press release how he originally became interested in this relationship after one of his own patients on an SGLT2 inhibitor was hospitalized for diabetic ketoacidosis, stating, “My best research projects come from my patients — their experiences drive the questions I investigate.”
“This is a side effect that’s usually seen in patients with type 1 diabetes mellitus – not type 2 – so doctors are not ‘on the lookout’ for it. That means that the risk of this side effect might actually be even higher than what we found due to misdiagnosis/under recording.”
The research group collected data on 50,220 patients with type 2 diabetes from the TruvenMarketScan database of commercially insured patients. All patients were started on an SGLT2 inhibitor or DPP4 inhibitor prior to the FDA warning (April 2013-December 2014).
“DPP4 inhibitors were chosen as the comparator medication because they are similarly used as a second-line treatment for diabetes but have no known association with diabetic ketoacidosis,” the authors wrote.
Utilizing a Cox regression model, Fralick’s group applied a 1:1 propensity-scare matching system to equally match participants based on 46 various characteristics to assess frequency of hospitalizations for diabetic ketoacidosis within 180 days of treatment initiation.
The research group also noted that patients who were prescribed SGLT2 inhibitors tended to be younger with fewer coexisting illnesses, although were more likely to be placed on insulin compared to patients on DPP4 inhibitors.
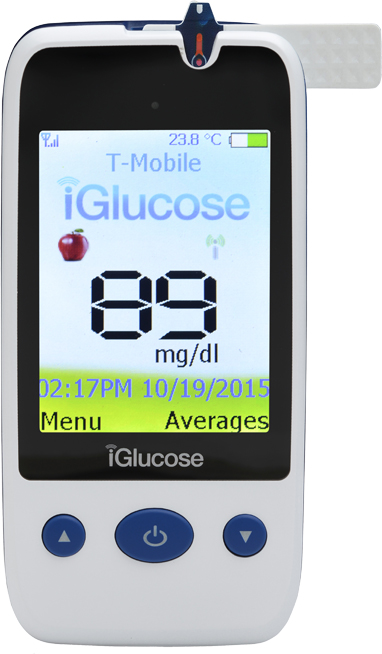
The researchers strongly suggest healthcare providers be vigilant for signs and symptoms of this in their patients, and should also be a factor to consider at time of prescription. In terms of prevention, Tamler added that he advises patients on SGLT2 inhibitors to “remain well-hydrated and stay on top of their blood sugar levels.”