The U.S. Food and Drug Administration (FDA) has approved XERAVA (Eravacycline), a fluorocycline antibacterial within the tetracycline class of antibacterial drugs, for the treatment of complicated intra-abdominal infections (cIAI) caused by susceptible microorganisms in patients 18 years of age and older.
XERAVA is not indicated for the treatment of complicated urinary tract infections (cUTI). To reduce the development of drug-resistant bacteria and maintain the effectiveness of XERAVA and other antibacterial drugs, XERAVA should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria.
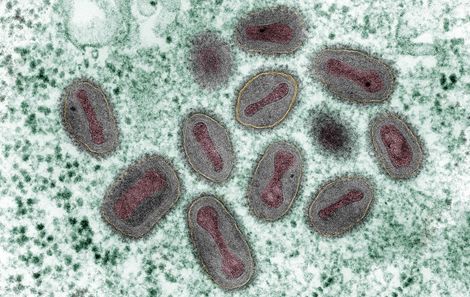
Susceptible microorganisms include: Escherichia coli, Klebsiella pneumoniae, Citrobacter freundii, Enterobacter cloacae, Klebsiella oxytoca, Enterococcus faecalis, Enterococcus faecium, Staphylococcus aureus, Streptococcus anginosus group, Clostridium perfringens, Bacteroides species, and Parabacteroides distasonis.
The approved recommended dosage of XERAVA is 1 mg/kg by intravenous infusion over approximately 60 minutes every 12 hours for a total duration of 4 to 14 days. The duration of therapy should be guided by the severity and location of infection and the patient’s clinical response. Additional information regarding dosage and administration can be found in the full prescribing information linked below.
Life-threatening hypersensitivity (anaphylactic) reactions have been reported with XERAVA.
is contraindicated for use in patients with known hypersensitivity to eravacycline, tetracycline-class antibacterial drugs, or to any of the excipients. Discontinue XERAVA if an allergic reaction occurs. The use of XERAVA may cause tooth discoloration and enamel hypoplasia, inhibition of bone growth, andclostridium difficile-associated diarrhea. Additional information regarding these important warnings can be found in the full prescribing information linked below.
Mechanism of Action (MOA) and Pharmacokinetics (PK)
- MOA: Eravacycline disrupts bacterial protein synthesis by binding to the 30S ribosomal subunit thus preventing the incorporation of amino acid residues into elongating peptide chains.
- General PK: Eravacycline AUC and Cmax increase proportionally over doses from 1 mg/kg to 3 mg/kg (3 times the approved recommended dosage). Accumulation is approximately 45% following the approved recommended dosage.
- Distribution: Protein binding of eravacycline increases with increasing plasma concentrations, with 79% to 90% (bound) at plasma concentrations ranging from 100 to 10,000 ng/mL. The volume of distribution at steady-state is approximately 321 L.
- Elimination: The mean elimination half-life is 20 hours.
- Metabolism: Eravacycline is metabolized primarily by CYP3A4- and FMO-mediated oxidation.
- Excretion: Following a single intravenous dose of radiolabeled eravacycline 60 mg, approximately 34% of the dose is excreted in urine and 47% in feces as unchanged eravacycline (20% in urine and 17% in feces) and metabolites.
Drug Interactions
CYP3A Inducers
Concomitant use of strong CYP3A inducers decreases the exposure of eravacycline, which may reduce the efficacy of XERAVA. Administer XERAVA 1.5 mg/kg every 12 hours for a total duration of 4 to 14days when used concomitantly with a strong CYP3A inducer. No dosage adjustment is warranted in patients with concomitant use of a weak or moderate CYP3A inducer.
Anticoagulant Drugs
Because tetracyclines have been shown to depress plasma prothrombin activity, patients who are on anticoagulant therapy may require downward adjustment of their anticoagulant dosage.
Use in Specific Populations
No clinically significant differences in the pharmacokinetics of eravacycline were observed based on age (18-86 years), sex, race, or renal impairment.
Patients with Hepatic Impairment
In patients with severe hepatic impairment (Child-Pugh C), administer XERAVA 1 mg/kg every 12 hours on Day 1, followed by XERAVA 1 mg/kg every 24 hours starting on Day 2 for a total duration of 4 to 14 days. No dosage adjustment is warranted in patients with mild to moderate hepatic impairment (Child-Pugh A and Child-Pugh B).
Efficacy and Safety
Efficacy of XERAVA was demonstrated in two Phase 3, randomized, double-blind, active-controlled, multinational, multicenter trials in adult patients hospitalized with cIAI. Additional information regarding efficacy trials can be found in the full prescribing information linked below.
The most common adverse reactions (incidence ≥ 3%) are infusion site reactions, nausea, and vomiting.
Full prescribing information available at www.accessdata.fda.gov