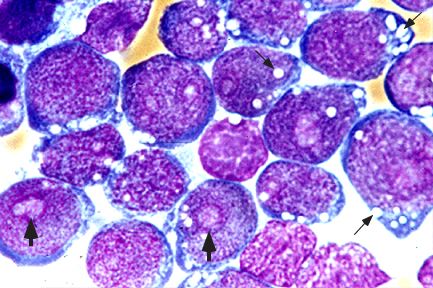
The FDA approved Kymriah (tisagenlecleucel) for certain pediatric and young adult patients with a form of acute lymphoblastic leukemia (ALL) that is refractory or has relapsed at least twice.
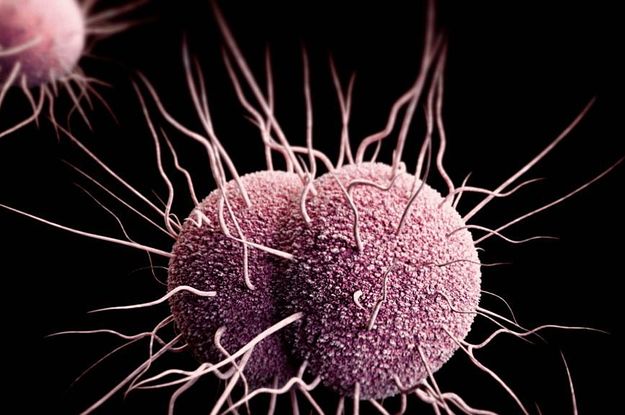
Novartis announced today that the US Food and Drug Administration (FDA) has approved Kymriah(TM)(tisagenlecleucel) suspension for intravenous infusion, formerly CTL019, the first chimeric antigen receptor T cell (CAR-T) therapy, for the treatment of patients up to 25 years of age with B-cell precursor acute lymphoblastic leukemia (ALL) that is refractory or in second or later relapse. Kymriah is a novel immunocellular therapy and a one-time treatment that uses a patient’s own T cells to fight cancer. Kymriah is the first therapy based on gene transfer approved by the FDA.
Kymriah is an innovative immunocellular therapy that is a one-time treatment. Kymriah uses the 4-1BB costimulatory domain in its chimeric antigen receptor to enhance cellular expansion and persistence. In 2012, Novartis and the University of Pennsylvania (Penn) entered into a global collaboration to further research, develop and commercialize CAR-T cell therapies, including Kymriah, for the investigational treatment of cancers.
Kymriah(TM) (tisagenlecleucel) Important Safety information
Kymriah may cause side effects that are fatal or life-threatening, such as Cytokine Release Syndrome (CRS) or Neurological Toxicities. Patients with CRS may experience symptoms including high fever, difficulty breathing, chills/shaking chills, severe nausea, vomiting and diarrhea, severe muscle or joint pain, very low blood pressure or dizziness/lightheadedness. Patients may be admitted to the hospital for CRS and treated with other medications.
Patients with neurological toxicities may experience symptoms such as altered or decreased consciousness, headaches, delirium, confusion, agitation, anxiety, seizures, difficulty speaking and understanding, or loss of balance. Patients should be advised to call their health care provider or get emergency help right away if they experience any of these signs and symptoms of CRS or neurological toxicities.
Because of the risk of CRS and neurological toxicities, Kymriah is only available through a restricted program under a Risk Evaluation and Mitigation Strategy (REMS) called Kymriah REMS.
Serious allergic reactions, including anaphylaxis, may occur after Kymriah infusion. Kymriah can increase the risk of life-threatening infections that may lead to death. Patients should be advised to tell their health care provider right away if they develop fever, chills, or any signs or symptoms of an infection.
Patients may experience prolonged low blood cell counts (cytopenia), where one or more types of blood cells (red blood cells, white blood cells, or platelets) are decreased. The patient’s health care provider will do blood tests to check all of their blood cell counts after treatment with Kymriah. Patients should be advised to tell their health care provider right away if they get a fever, are feeling tired, or have bruising or bleeding.
Patients may experience hypogammaglobulinemia, a condition in which the level of immunoglobulins (antibodies) in the blood is low and the risk of infection is increased. It is expected that patients may develop hypogammaglobulinemia with Kymriah, and may need to receive immunoglobulin replacement for an indefinite amount of time following treatment with Kymriah. Patients should tell their health care provider about their treatment with Kymriah before receiving a live virus vaccine.
After treatment with Kymriah, patients will be monitored life-long by their health care provider, as they may develop secondary cancers or recurrence of their leukemia.
Patients should not drive, operate heavy machinery, or do other dangerous activities for 8 weeks after receiving Kymriah because the treatment can cause temporary memory and coordination problems, including sleepiness, confusion, weakness, dizziness and seizures.
Some of the most common side effects of Kymriah included: difficulty breathing, fever (100.4°F/38°C or higher), chills/shaking chills, confusion, severe nausea, vomiting and diarrhea, severe muscle or joint pain, very low blood pressure, and dizziness/lightheadedness. However, these are not all of the possible side effects of Kymriah. Patients should talk to their health care provider for medical advice about side effects.
Prior to a female patient starting treatment with Kymriah, their health care provider may do a pregnancy test. There is no information available for Kymriah use in pregnant or breast-feeding women. Therefore, Kymriah is not recommended for women who are pregnant or breast feeding. If either sex partner has received Kymriah, patients should talk to their health care provider about birth control and pregnancy.
Patients should tell their health care provider about all the medicines they take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
After receiving Kymriah, patients should be advised that some commercial HIV tests may cause a false positive test result. Patients should also be advised not to donate blood, organs, or tissues and cells for transplantation after receiving Kymriah.